Wayne Lowry

Why is direct primary care growing? Direct primary care (DPC) is a healthcare model where patients pay a monthly fee directly to their primary care provider, bypassing traditional insurance. This model is gaining traction due to several reasons:
With the rise of direct primary care, patients and providers are rethinking what healthcare can look like.
At its heart, direct primary care represents a shift in healthcare delivery, emphasizing a strong patient-provider relationship and prioritizing primary care. This model is not just about breaking away from insurance woes but also about restoring the core values of medical care. It allows doctors and patients to connect more deeply, focusing on health rather than billing.
Doctors can provide better care since they aren’t overwhelmed with paperwork, and patients get the attention they need. This makes healthcare feel personal again—a big reason why DPC continues to grow.
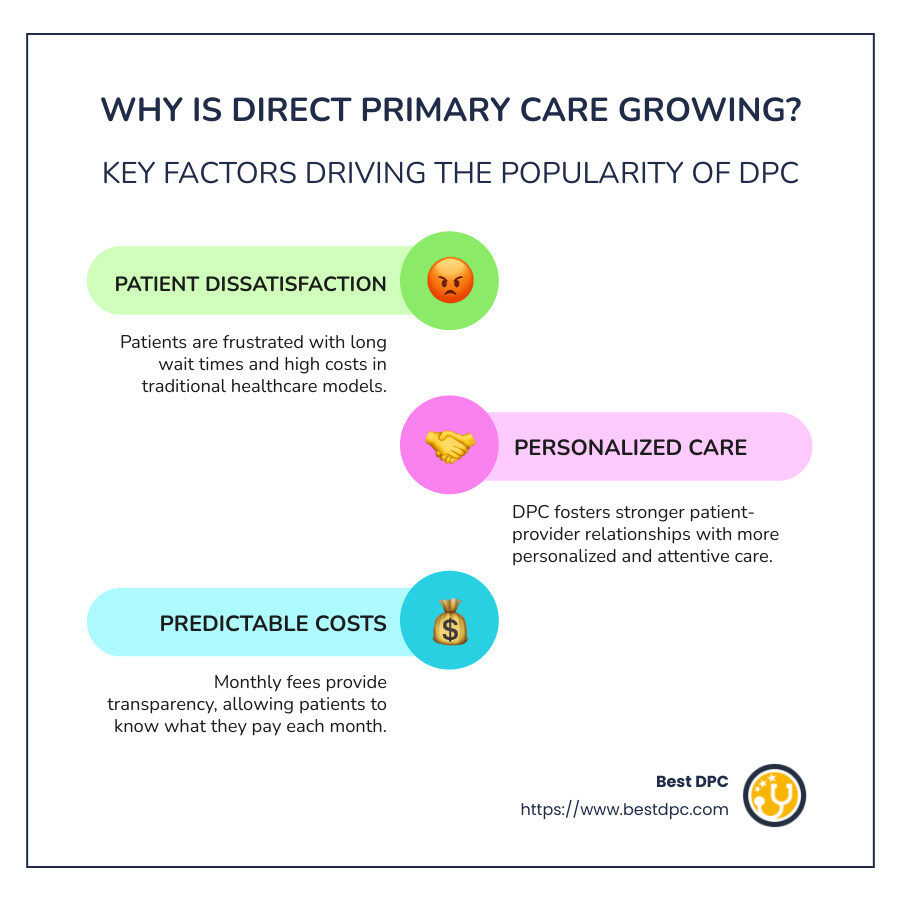
Why is Direct Primary Care Growing?
Direct primary care (DPC) is becoming more popular, and there are a few key reasons why. Let’s explore them:
Patient Dissatisfaction
Many patients feel frustrated with the traditional healthcare system. Long wait times, rushed appointments, and confusing bills are common complaints. According to a recent study, there’s a growing desire for a system that prioritizes patient needs over paperwork. DPC addresses these issues by offering longer appointments, same-day visits, and transparent pricing. Patients know exactly what they’re paying for, which can be a big relief.
Physician Autonomy
Doctors are also seeking change. In traditional settings, many physicians feel bogged down by administrative tasks and insurance hassles. This can lead to burnout and dissatisfaction. DPC offers doctors the freedom to focus more on patient care and less on paperwork. Many doctors report feeling like they’re practicing the best medicine of their careers. They enjoy having more control over their schedules and the ability to build stronger relationships with their patients.
Personalized Care
DPC allows for a more personalized approach to healthcare. Doctors can spend more time with each patient, getting to know them and their health needs better. This focus on personalized care leads to better health outcomes and a more satisfying experience for both patients and doctors. Patients appreciate being treated as individuals, not just numbers or cases. This approach fosters trust and encourages patients to be more engaged in their health.
The rise of DPC is fueled by a desire for a more patient-centric and doctor-friendly healthcare model. It’s about making healthcare more accessible, personal, and efficient for everyone involved.
Benefits of Direct Primary Care
Direct primary care (DPC) brings several benefits that make it an attractive option for both patients and physicians. Let’s explore these key advantages:
Cost-Effectiveness
DPC is known for its affordability. Patients pay a flat monthly fee, which covers most primary care services without additional costs like co-pays or deductibles. This predictable pricing helps patients avoid unexpected medical bills. By eliminating insurance claims and reducing administrative costs, DPC practices can offer more affordable care. This model is especially beneficial for individuals managing long-term health conditions, as it minimizes out-of-pocket expenses for routine visits and chronic care management.
Improved Access
Access to healthcare is a major concern for many. DPC improves access by providing longer appointments and same-day or next-day visits. Patients can also communicate directly with their doctors via phone or email, ensuring timely and personalized attention. This level of access is a significant improvement over traditional systems, where patients often face long wait times. In urban and suburban areas, where demand for innovative healthcare solutions is high, DPC practices have flourished.
Preventive Care
Preventive care is a cornerstone of DPC. By focusing on early detection and management of health issues, DPC reduces the long-term costs and complications associated with chronic diseases. Patients are more likely to engage in routine care and early intervention, leading to better long-term health outcomes. This emphasis on prevention aligns with a growing public awareness of the importance of maintaining health and wellness.
Reduced Administrative Burden
For physicians, one of the most appealing aspects of DPC is the reduced administrative burden. Traditional healthcare systems often require doctors to spend significant time on paperwork and insurance-related tasks. DPC eliminates these hassles, allowing doctors to focus on patient care. This reduction in administrative duties not only improves physician satisfaction but also improves the quality of care patients receive. Physicians report feeling more fulfilled and able to practice medicine as they envisioned when they chose their careers.

In summary, DPC offers a cost-effective, accessible, and preventive approach to healthcare while reducing the administrative tasks that often burden physicians. This model is gaining popularity for its ability to provide comprehensive and personalized care, benefiting both patients and doctors.
Challenges and Opportunities in Direct Primary Care
Direct primary care (DPC) is growing rapidly, but it faces several challenges and opportunities that could shape its future.
Misconceptions
A challenge for DPC is overcoming misconceptions about its model. Many people confuse DPC with concierge medicine, but they are different. DPC offers affordable, accessible care without relying on insurance billing. Educating patients and healthcare providers about these differences is crucial for DPC’s continued growth.
State Laws
State laws can also pose challenges for DPC practices. Regulations vary widely, affecting how DPC models operate in different regions. Some states have more favorable laws that support DPC, while others have restrictions that can make it difficult for practices to thrive. Advocating for supportive legislation is an ongoing effort for DPC advocates.
Chronic Disease Management
DPC presents significant opportunities in chronic disease management. By offering longer appointments and more direct communication with doctors, DPC helps manage chronic conditions more effectively. Patients receive personalized care plans, which can lead to better health outcomes and reduced healthcare costs over time. This model is particularly beneficial for patients with complex medical needs, who require consistent and coordinated care.
Physician Satisfaction
Physician satisfaction is a key opportunity that DPC offers. Many doctors are drawn to DPC because it allows them to focus more on patient care and less on administrative tasks. This satisfaction not only improves doctors’ work-life balance but also improves the quality of care they provide.
The Role of Technology in Direct Primary Care
Technology plays a pivotal role in enhancing the direct primary care (DPC) model, making healthcare more efficient and patient-centered. Let’s explore how telehealth, electronic health records (EHRs), and personalized medicine contribute to the growth and success of DPC.
Telehealth
Telehealth is revolutionizing how patients access care, particularly in DPC practices. By enabling remote consultations, telehealth breaks down geographical barriers, allowing patients to connect with their doctors from the comfort of their homes. This is especially beneficial for those in rural areas where access to healthcare can be limited.
Telehealth also provides flexibility for both patients and physicians, reducing the need for in-person visits for minor consultations. This convenience results in more timely care and helps maintain strong patient-provider relationships.
Electronic Health Records
Electronic Health Records (EHRs) are another technological advancement that supports DPC’s mission of providing personalized care. EHRs streamline patient data management, making it easier for physicians to access comprehensive medical histories and tailor treatment plans accordingly.
In DPC, where the focus is on long-term health and prevention, EHRs are invaluable. They allow for better tracking of patient outcomes and facilitate seamless communication between healthcare providers, ensuring coordinated and effective care.
Personalized Medicine
Personalized medicine is an emerging trend in DPC that leverages technological advancements to tailor healthcare to individual patients. This approach includes using genetic testing and other diagnostic tools to create customized treatment plans.
By integrating personalized medicine, DPC practices can offer more precise and effective care, improving patient outcomes and satisfaction. This innovation aligns with the DPC model’s emphasis on individualized attention and proactive health management.

Incorporating technology into DPC not only improves the efficiency and quality of care but also strengthens the patient-provider relationship. As technology continues to evolve, its role in DPC will likely expand, offering even more opportunities to improve healthcare delivery.
Next, we’ll address some frequently asked questions about Direct Primary Care.
Frequently Asked Questions about Direct Primary Care
What is Direct Primary Care?
Direct Primary Care (DPC) is a healthcare model where patients pay a monthly fee directly to their primary care provider. This fee covers most or all primary care services, eliminating the need for traditional insurance. Patients enjoy unlimited access to their physician, including routine check-ups, preventive care, and urgent visits, without the hassle of insurance billing or co-pays.
This model focuses on simplicity and accessibility, offering patients more personalized care and fostering a stronger patient-provider relationship.
How does Direct Primary Care differ from traditional models?
In traditional healthcare models, fee-for-service is the norm. Here, each visit or service is billed separately, often involving complex insurance billing processes. This can lead to brief, rushed interactions between patients and physicians, as doctors juggle administrative tasks and insurance constraints.
In contrast, DPC emphasizes longer patient interactions and personalized care. With no insurance middlemen, physicians can focus more on patient needs rather than paperwork. This results in better care, as doctors have the time to understand and address their patients’ health concerns comprehensively.
What are the potential risks of Direct Primary Care?
While DPC offers many benefits, there are potential risks to consider:
Despite these challenges, many physicians find the DPC model rewarding, as it allows them to practice medicine on their terms and prioritize patient care.
Next, we’ll dig into the benefits of Direct Primary Care and how it can transform healthcare for both patients and providers.
Conclusion
Direct Primary Care (DPC) is reshaping healthcare by prioritizing patient-centered care. At its core, DPC focuses on fostering strong relationships between patients and providers, offering personalized attention and eliminating the complexities of insurance.
Best DPC plays a crucial role in this change by connecting patients with dedicated DPC providers. Their approach emphasizes affordability and accessibility, making quality healthcare available to a broader audience. This model not only benefits patients but also empowers physicians by allowing them to focus on delivering the best care possible.
The future of healthcare lies in innovative models like DPC. As the industry evolves, DPC is expected to expand further, integrating more with specialty care and leveraging technology to improve patient experiences. This growth is driven by a shared commitment to improving health outcomes and making healthcare more efficient and effective.
By embracing DPC, healthcare providers can offer a more satisfying experience for both patients and themselves. This model represents a significant shift towards a more compassionate and patient-focused healthcare system.
Explore how Best DPC is leading the way in delivering personalized healthcare solutions.

ABOUT AUTHOR
Wayne Lowry
Wayne Lowry, Founder of BestDPC, is a passionate advocate for Direct Primary Care (DPC) and its mission to deliver personalized, accessible healthcare. He believes that DPC providers should serve as the trusted first point of contact for all medical needs, ensuring patients never feel isolated or uncertain about their health decisions. Through his work, he champions a patient-first approach to healthcare, building a system that prioritizes guidance, support, and trust.

Thank You for Registering!
Your registration was successful! We're excited to have you on board. Please check your email for a confirmation link to complete your registration.